North America is a region with a lot of diabetes. In certain estimates across the region, up to 10% of the population suffers from this disease. Unfortunately, all of us are quite used to seeing people treated for high blood glucose, and also to seeing the results of the terrible complications that appear after many years, sometimes even in close relatives.
No system within the body is spared from the damage secondary to excess sugar in the bloodstream. As we have all seen, it affects the nerves, the immune system, the skin, the gastrointestinal system, the liver, the kidneys, the heart, the lungs, and of course, the eyes.
The ocular complications of diabetes are the first cause of blindness in the population of 20-50 years, that is, people in economically active age. Therefore, it is important to understand the mechanisms behind the damage, because that way it is easier to comply with treatment, and prevent irreversible vision loss.
The most important thing to visualize is that diabetes affects all the structures within the body because it is a disease of the blood vessels. It is those little hoses that carry blood with an excess of sugar all throughout the body, that are responsible for the cumulative damage. The reason is that glucose is a substance that generates oxidation, and when it is present in excess, the internal walls of the blood vessels start to exhibit a breakdown related to this oxidation. First the smallest vessels, called capillaries, and gradually, larger ones called arterioles, but ultimately, also the major arteries.
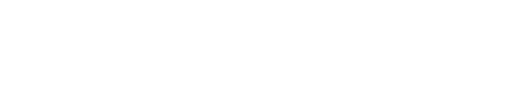
The retina, which sits on the inner walls of the eye, is a tissue that uses a lot of oxygen to convert light into stimuli which the brain is able to read. All the time we are awake, it is working non stop, which means that its oxygen and nutrient expenditure is quite high. Therefore, it is provided with many many blood vessels, of all sizes (image 1).

The abundance of these vessels explains why the retina is so sensitive to diabetes, and as a matter of fact, what is found in the rest of the body when blood sugar is out of control, is what we see in the office upon pupil dilation and direct retinal examination.
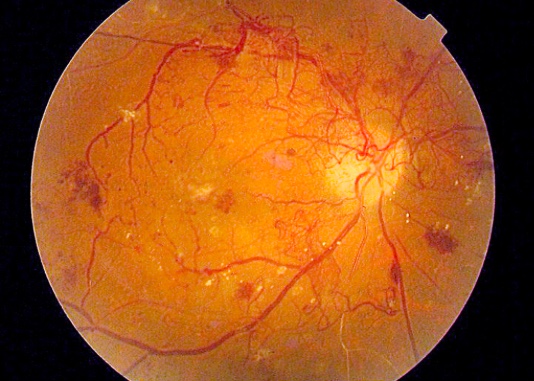
The first sign of diabetes-related damage is the appearance of small dilations in the thinnest capillaries, which start resembling small balloons filled with blood, called microaneurysms. Later in the process, larger vessels become affected as well, and develop leaks, which flood the retina with liquid and generate inflammation. If the disease is not controlled, parts of the retina undergo infarction (lack of oxygen) because there is no longer a way to bring it there (Image 2).

When large areas of the retina are deprived of oxygen, a substance is produced, which “asks the body” to construct new blood vessels and therefore quench the need for nutrients. The body acts in consequence, and develops new capillaries and arterioles, trying to compensate. However, these new vessels are fragile, and often tear, causing large hemorrhages. This is the reason why patients with advanced diabetes sometimes lose vision in a sudden way.
Additionally, these new vessels or “neovascularization”, grow along a membrane that tends to contract in time, like scar tissue, and cause the retina to be detached from its place, resulting in loss of function, and therefore, of vision (Image 3).

The lines written above explain the causes of vision loss in diabetes, also known as diabetic retinopathy (retinal disease due to diabetes, in medical language). The subsequent article will deal with the treatment strategies for each of the levels of damage, but I will leave you with a spoiler: The most important, by far, in the treatment of diabetic retinopathy, is The control of blood glucose levels.
Thank you very much for your attention.
Dr. Victor Flores.